- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Humanitarian Assistance
- Transformation at USAID
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab
Speeches Shim

At a Glance
- Introduction
- I. Interventions to Deliver Micronutrients
- II. Selecting One or More Micronutrient Interventions
- Conclusion
- References
- Footnotes
View the PDF [PDF, 461KB].
Introduction
Box 1. Global Burden of Disease
- Vitamin A deficiency, resulting in clinical symptoms, affects approximately 10 million pregnant women and 5 million children.
- Prevalence of iron deficiency anemia ranges from 11 percent to 16 percent for preschool children and 10 percent to 15 percent for pregnant women.
- Zinc deficiency affects approximately 17 percent of the world’s population.
- Iodine deficiency disorders are kept under control in most countries of the world through the addition of iodine to salt and salt-containing products* (Black, 2014).
* Without these interventions, billions of people worldwide would have inadequate intake of iodine.
This brief provides an overview of effective ways to deliver essential vitamins and minerals, collectively called micronutrients, to populations. The descriptions of advantages and limitations of different micronutrient approaches can help program managers select the appropriate micronutrient program to prevent and correct insufficient micronutrient intakes for a target population based on the country context. Insufficient micronutrient intake, often referred to as micronutrient inadequacy, results from the lack of consumption of foods that supply those micronutrients. Micronutrient inadequacy is one of the causes of micronutrient deficiency; other causes of this deficiency are micronutrient losses due to diseases and infections, parasitism and even genetic abnormalities. Micronutrient deficiencies remain widespread and disproportionately affect vulnerable sub-groups within populations (see Box I).
The food fortification and supplementation approaches described in this brief can correct for inadequacies and can help reduce the consequences of micronutrient deficiencies. Other approaches, such as infection prevention and treatment, also reduce micronutrient deficiencies, but these approaches will not be covered in this brief.
Micronutrient deficiencies are frequently known as “hidden hunger” because the symptoms of deficiency often manifest only when they become severe, yet the consequences of mild or moderate deficiency – frequently not detected – have large health, social and economic impacts on individuals and their communities (see Box 2).
A significant proportion of the global burden of micronutrient deficiencies is concentrated in sub-Saharan Africa and South Asia (see Figure 1). This geographic concentration exists for many reasons, including poor dietary diversity due to poverty and food insecurity, low bioavailability of nutrients in diets and nutrient loss due to illness. The long-term solution for solving micronutrient inadequacies is using food-based approaches to ensure a diverse, sustainable and nutritious diet, which may be complemented with food fortification and, for specific life-stages and population groups, micronutrient supplementation to ensure supply of micronutrients that might be insufficient in the usual diets (Mayo-Wilson, et al., 2011; Peña-Rosas, et al., 2012).
Box 2. Negative Consequences
- Vitamin A deficiency often results in night blindness, and it may affect eye health and child survival.
- Iron deficiency during the fetal period and early childhood can significantly impair child growth and mental development.
- Iodine deficiency during pregnancy and the first years of life can cause permanent physical, mental and cognitive damage.
- Zinc deficiency damages the immune system and may contribute to childhood stunting.
- Folate and vitamin B12 deficiencies in early pregnancy can lead to devastating fetal neural tube defects.
- Vitamin D and calcium deficiencies cause rickets and growth retardation in children as well as osteoporosis and osteopenia (weak bones) in adults. In addition, vitamin D deficiency is associated with increased risk of common cancers, autoimmune diseases and hypertension (WHO & FAO, 2004).
The benefits of treating and preventing micronutrient deficiencies are well documented. Vitamin A supplied through supplements, for example, can prevent child blindness and reduce mortality in children aged 6 months to 5 years old by 23 percent (Mayo-Wilson, et al., 2011). Anemia, including that caused by iron deficiency, can contribute to postpartum hemorrhage and is a suspected contributor to maternal mortality in about 20 percent of maternal deaths. Iron supplementation in pregnancy prevents low birthweight, maternal anemia and other adverse outcomes due to iron deficiency (Peña-Rosas, et al., 2012). The Copenhagen Consensus in 2008 identified micronutrient interventions as top priority actions for improving human health and wellbeing (Horton, Mannar, & Wesley, 2008). In May 2012, the third Copenhagen Consensus further concluded that “bundled interventions to reduce undernutrition in pre-schoolers” should be the main priority for international development, which puts a further focus on public health strategies that can tackle micronutrient deficiencies (Copenhagen, 2012). This brief is divided into two sections: an overview of interventions to deliver micronutrients and guidance on the decision-making process when selecting an intervention.
Figure 1. Map of Worldwide Distribution of Anemia, and Vitamin A and Zinc Deficiencies
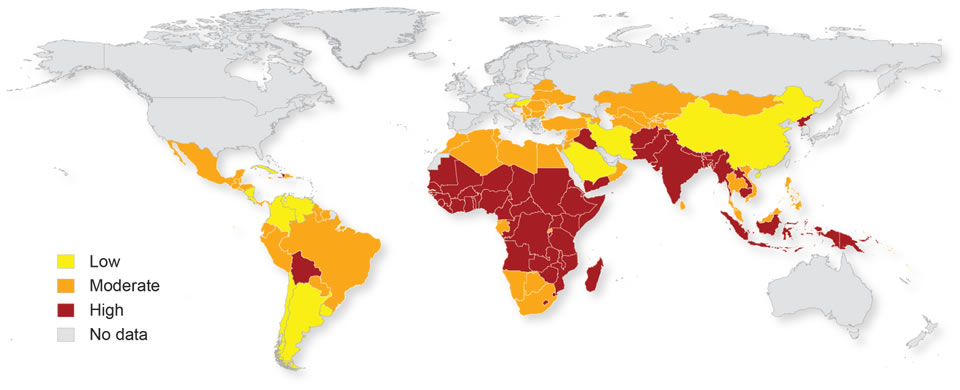
This map details worldwide severity of anemia (as a sign of several micronutrient deficiencies) – and vitamin A and zinc deficiencies – using World Health Organization (WHO) children under 5 prevalence data. Severity was coded using a 3-point weighting system based on levels of public health significance cutoffs (low, moderate and high). The cutoffs for each deficiency are anemia (<5% no public health problem; 5-19.9%-mild public health problem; 20-39.9%-moderate public health problem; ≤40%-severe public health problem); vitamin A (population prevalence of low serum retinol <0.7 µmol/L ≥ 10%, of night blindness >1%, of Bitot’s spots >0.5%, of corneal xerosis and/or ulceration >0.01% or of xerophthalmia related corneal scars >0.05%); and zinc (indicator is low height-for-age or stunting among under-5 children and public health significance is classified as low ≤20 %, moderate >20–40% or high ≥40%). These cutoffs are weighted to give the final 3-point scale of low, moderate and high (HarvestPlus, 2012).
I. Interventions to Deliver Micronutrients
Interventions to deliver micronutrients fall under five broad categories: nutrition-sensitive approaches, dietary diversification and modification, breastfeeding, fortification of food with micronutrients and the provision of vitamin and mineral supplements to targeted populations (Box 3).
Box 3. Interventions to Deliver Micronutrients
- Agricultural approaches
- Dietary diversification and modification
- Breastfeeding
- Food fortification
- Mass fortification
- Targeted fortification
- Fortified blended foods (FBF)
- Ready-to-use therapeutic food (RUTF)
- Ready-to-use supplementary foods (RUSF)
- Commercial-driven fortification
- Supplementation
- Traditional supplementation programs
- Point-of-use “fortification”
Agricultural Approaches
Nutrition-sensitive activities and interventions address the underlying and systematic causes of malnutrition. They influence outcomes related to food security; adequate caregiving resources at the maternal, household and community levels; healthy timing and spacing of pregnancies; and a safe and hygienic environment. Agriculture is one of the key sectors through which nutrition-sensitive activities can be implemented, and these activities should be programmed along with nutrition-specific actions, or that address the immediate determinants of malnutrition.
Nutrition-sensitive agriculture interventions play a key role in improving the nutritional status of women and children. While increased production and productivity can increase the availability of food for consumption, increase incomes and decrease the prices consumers pay, these alone do not automatically translate to nutritional gains. Nutrition-sensitive agriculture interventions can increase the availability and consumption of diverse and nutritious foods for rural households, especially for women and children, via three main pathways:
- Food Production – to increase the availability and affordability of nutrient-rich foods for household consumption
- Income – to increase expenditure on food and non–food items
- Women’s Empowerment – to increase women’s decision-making power over use of income, feeding and caregiving practices and efficient female energy expenditure (Herforth & Harris, 2014)
Interventions that contribute to making safe, micronutrient-rich foods more available and accessible to low-income consumers can improve dietary diversity and nutrient intake. Entry points for nutrition-sensitive interventions, such as homestead food production or livestock-oriented programs that include social and behavior change activities, are outlined in USAID’s Nutrition-Sensitive Agriculture: Nutrient-Rich Value Chains technical brief.1
To achieve nutrition goals, nutrition-sensitive interventions should be carefully designed to promote gender equality and women’s empowerment. Approaches should engage both women and men to bring about changes in attitudes, roles and behaviors. Women’s time, control of income and care-giving and labor demands should be considered when designing interventions to prevent overburdening women or negatively impacting the health of women and children (see USAID’s Nutrition-Sensitive Agriculture: Applying the Income Pathway technical brief 2 for more information on considerations and approaches).
In addition, biofortification – which involves increasing the micronutrient content of common crops and their bioavailability – can be a good strategy to increase micronutrient intake. Promising reports exist of increased iron and zinc supplies with biofortified pearl millet (Kodkany, et al., 2013) and common beans (Petry, et al., 2014) as well as vitamin A contents in biofortified orange-fleshed sweet potatoes (Hotz, et al., 2012). The integration of biofortified crops into agricultural value chains and food systems requires enhanced efforts to increase the production, acceptability and processing of these crops. These efforts, alongside efforts to create consumer desirability for such products, will ensure that biofortified crops are readily available and affordable in local markets throughout the year.
Dietary Diversification and Modification
In most resource-poor settings, diets are mainly comprised of starches, as individuals consume limited quantities of meats, eggs, dairy, fruits and fresh vegetables. However, improving household diets requires an increase in the presence of these foods in the diet.
Dietary diversification refers to interventions that increase the variety of foods consumed at the household level, such as increasing consumption of animal-source foods (Gibson & Anderson, 2009; Gibson, Perlas, & Hotz, 2006). Incorporating animal-source foods, either fresh or in dried form, increases the availability of vitamin A, iron, zinc and vitamins B2 and B12 in the diet (Gibson, 2014).
Dietary modification involves changes in food preparation, processing and consumption at the commercial, individual or household level to enhance the bioavailability of micronutrients in food. For example, coffee and tea contain polyphenols, which inhibit iron absorption, so their consumption alongside food at meal times should be discouraged.
Food can be processed to improve bioavailability by employing processes such as germination, fermentation and soaking to reduce the phytate content that can interfere with absorption of iron and zinc. These practices have resulted in improvements in iron and zinc status, although this effect is not always detected (Gibson, Perlas, & Hotz, 2006). On an individual level, however, these practices can make incremental improvements in the intake and absorption of micronutrients and are advantageous due to their cultural acceptability and economic feasibility (Gibson, 2014). For these strategies to be successful, they have to be integrated into other household practices or be applied by the food industry.
Before introducing dietary diversification or modification, formative research should be conducted to understand food habits at the household and individual levels and access to foods along with the social and cultural barriers and opportunities that influence diet. Information that could be helpful includes dietary patterns, nutrient intakes and diets of individuals and households; cost of the food basket based on current consumption, economic indicators and food costing data; and information on the knowledge, attitudes, beliefs and practices of the family about the importance of vitamins and minerals in food (Gibson, 2014).
Making changes to household dietary practices requires a behavior change approach; strategies that have been shown to impact dietary practices include active nutrition education, counseling and social marketing campaigns to communicate the benefits associated with making changes to dietary practices (Guldan, et al., 2000).
Additionally, strategies must address the availability and affordability of a safe diet year-round, as these factors can constrain households’ abilities to improve dietary practices. Dietary diversification and modification can address multiple micronutrient inadequacies simultaneously and reach each household member’s varying dietary needs. That said, in resource-poor settings, a dietary strategy is unlikely to fully meet all nutritional needs, and additional strategies, such as fortification and supplementation, should also be considered (Torheim, et al., 2010).
Breastfeeding
Human milk is the ideal, sole source of nutrition for children younger than 6 months of age and an optimal complement to the diet through the second year of life. WHO recommends exclusive breastfeeding until 6 months of age, with continued breastfeeding along with appropriate complementary foods until the second year of life or longer. Breastfeeding protects children against infection and is critical to the mental and physical wellbeing of babies and their mothers (Lönnerdal, 1985).
The content of some micronutrients in breast milk is dependent on maternal intake and on the mother’s micronutrient status. The breast milk concentration of some water-soluble vitamins like thiamin (B1), riboflavin (B2), pyridoxine (B6), niacin (B3), vitamin B12 and ascorbic acid (C) is responsive to maternal intake, while that of folate is not unless the mother is severely deficient. Among the fat-soluble vitamins, increased maternal intake of vitamin A and vitamin D can lead to increased levels in breast milk. Likewise, among minerals, consumption of foods or products with iodine and selenium increases the content of these minerals in breast milk, but this is not true for iron, zinc and copper (Allen, 2005). The content of calcium in breast milk is adequate, and it comes from the mother’s bones.
From a program perspective, interventions that improve the nutritional status of all adolescent girls and women of reproductive age are the best approaches to ensure that women maintain adequate micronutrient stores during pregnancy and lactation.
Food Fortification
Food fortification is the addition of one or more essential nutrients to an industry-manufactured food, whether or not they are normally contained in the food, for the purpose of preventing or correcting a demonstrated deficiency of one or more nutrients in the population or specific population groups (WHO and FAO, 2015). There are three main types of food fortification: (i) mass fortification refers to the addition of micronutrients and minerals to commonly eaten products, such as cereal staples, rice, oil, sugar, milk and salt; (ii) targeted fortification refers to the addition of micronutrients to certain foods that a specific population or age group consumes, for example, emergency rations for refugees or complementary foods for children in preschool feeding programs; and (iii) commercial-driven fortification refers to when food manufacturers fortify their product with micronutrients to enhance its marketability, which sometimes may have positive influence in the diet, for example the addition of vitamin D and calcium to orange juice (WHO and FAO, 2006). Fortification is less expensive than dietary diversification and supplementation if the food is manufactured by relatively well-developed and centralized industries.
I. Mass Fortification (edible products with wide consumption)
Mass fortification should be considered when micronutrient inadequacy is widespread and appropriate conditions are available for the production, sale, standard enforcement, and monitoring of fortified products. The most commonly fortified foods are staple foods, such as corn flour, wheat flour and rice; vegetable oil; sugar; milk; and salt. The choice of foodstuff to fortify (industry-made and widely consumed by the target population) and the formulation of the premix/fortificants (for filling the micronutrient gaps) are two of the most important decisions to make when considering mass fortification.
The universal salt iodization program is the classic example of a successful, large-scale public health fortification program (Andersson, Vallikannu, & Zimmermann, 2012). Other examples of fortification include folic acid in flour (Hertrampf, et al., 2003) and vitamin A in cooking oil and sugar (von Grebmer, et al., 2014; Fiedler & Lividini, 2014; Fiedler, Lividini, & Bermudez, 2015; Arroyave, Mejía, & Aguilar, 1981). Fortification of foods with multiple vitamins and minerals has been shown to improve iron and vitamin A status as well as to reduce anemia (Eichler, Weiser, Rüthemann, & Brügger, 2012; Martorell, et al., 2015).
Successful mass fortification requires government regulation and enforcement. It also includes quality control and assurance procedures for the manufacturing industry. An existing production facility as well as an ongoing production process and supply chain enable easy and cost-efficient industrial production and trade of the fortified product. If the conditions are not appropriate – for example, production of milled flours is through small and underdeveloped cottage industries – other interventions for the delivery of micronutrients should be considered instead of fortification.
It is important to note that mass fortification does not involve promoting the consumption of these fortified food vehicles. Effective mass fortification builds on, rather than changes, the normal eating habits of the population; social marketing is therefore often not necessary. Efforts to prevent non-communicable diseases frequently aim to reduce the consumption of typical vehicles for food fortification such as salt, sugar and oil. Mass fortification is compatible with these efforts; fortified foods are only used as delivery vehicles, and the micronutrient content can be adjusted to changing intake patterns.
Mass fortification has the advantage of reaching large sections of the population through markets. However, this method may only partially benefit those whose micronutrient requirements are higher than the needs of the general population, such as young children or pregnant and lactating women. For those whose needs are not fully met, it is useful to use targeted fortification or supplementation to complement mass fortification.
II. Targeted Fortification (addition of micronutrients to food for specific populations)
In targeted fortification, the objective is to develop special foods that meet the micronutrient needs of specific populations or age groups. The World Food Programme (WFP) uses targeted fortification in complex emergencies where markets may not be functioning to support mass fortification or other interventions (Nutrition Service, 2006). The WFP often provides food rations that are designed to meet the macronutrient and micronutrient needs of the population through the provision of fortified-blended foods (FBF). These are frequently targeted to pregnant and lactating women and young children. Outside of humanitarian settings, several other examples of targeted fortification with multiple micronutrients exist, including Incaparina – a fortified blended flour made with corn and soy flours in Guatemala; other blended flours used as complementary foods for infants in Indonesia; – a blended flour used as complementary food in Peru (WHO and FAO, 2006).
In humanitarian assistance, several FBFs are used, such as corn-soy blend plus (CSB+)3 or wheat-soy blend (WSB), which contain corn or wheat, soybeans, sugar, vegetable oil and a micronutrient premix, as well as Super Cereal Plus (CSB++), which adds dried milk powder to the other ingredients in CSB+. Evidence shows that the use of fortified complementary foods improves micronutrient intakes, with positive effects on iron and vitamin A status, two micronutrients that have been measured in various studies (Dewey & Adu-Afarwuah, 2008).
Two other food formulations may also fall under the category of targeted fortification vehicles: Ready-to-Use Therapeutic Foods (RUTF) and Ready-to-Use Supplementary Foods (RUSF), which are mostly in the form of Lipid-based Nutrient Supplements (LNS). These products are dense in both energy and protein, and they supply essential fatty acid and micronutrients to meet the needs of individuals who are malnourished (Gibson, 2014).
RUTFs are used to treat uncomplicated cases of severe acute malnutrition (SAM) in an outpatient setting. Its concentrated formulation stipulates recovery for severely wasted individuals. Modifications of this product and reduction in serving size led to RUSFs, which are used for the prevention and treatment of moderate acute malnutrition (MAM). RUSF is meant for use as a supplementary food, intended to prevent severe acute malnutrition and stimulate recovery of moderate wasting when supplementing the local diet. Table 1 summarizes FBF, RUSF and RUTF use in humanitarian assistance programs (Webb, et al., 2011).
Table 1. Use of Fortified Blended Foods (FBF) and Ready-to-use Foods (RUTF/RUSF)
|
Product |
Age Group |
Micronutrients |
Uses |
|
FBF – CSB Plus, WSB, Super Cereal Plus, etc. |
|
Minerals: calcium, iron, zinc, copper, magnesium, manganese, phosphorus, selenium, and iodine Vitamins: folate, thiamin, riboflavin, niacin, pantothenic acid, pyridoxine, vitamins A, B12, D3, and E |
|
|
RUSF |
|
Multiple micronutrients as in FBF, plus vitamins K and C and potassium |
|
|
RUTF |
|
Multiple micronutrients as in FBF, plus vitamins K and C and potassium |
|
III. Commercial-driven Fortification
Commercial, or market-driven, fortification is when food manufacturers add one or more micronutrients to a specific food product for a business or brand advantage. When the manufacturer of the food product makes a business decision to fortify, it may have a positive impact on the population’s micronutrient supply if the product’s content and marketing are appropriately regulated. Examples of commercial-driven fortification products include fortified breakfast cereals and beverages. These processed products typically reach a smaller portion of the population than those reached by fortified staple foods, and many times they do not reach the most vulnerable groups in the population.
Government regulation is always necessary to ensure that the fortification of processed foods or beverages will not lead to undesirably high intakes of micronutrients, a possibility when products are over-fortified or when individuals consume a variety of fortified products. Moreover, marketing of these products should also be checked to respond to public health interests.
Supplementation
According to the U.S. Food and Drug Administration, a supplement is a product that contains a dietary ingredient intended to add further nutritional value to the diet. Supplement formulations include tablets, capsules, softgels, gelcaps, liquids or powders (FDA, 2015). Supplements could be consumed alone or together with foods. In public health, there are two main strategies for the use of micronutrient supplements: traditional supplementation programs and point-of-use “fortification.”
1. Traditional Supplementation Programs
Supplementation should be targeted to vulnerable groups whose micronutrient needs are not adequately met from food sources alone. Pregnant women are commonly targeted for supplementation by traditional pharmaceutical preparations as their micronutrient needs are increased during pregnancy. Iron and folate requirements are higher during pregnancy, and these two micronutrients are usually provided during this stage to prevent maternal anemia, reduce the risk of low birthweight and improve iron status of both the mother and the newborn (Imdad, Yakoob & Bhutta, 2011; WHO and FAO, 2004). Supplementation with iron and folic acid (IFA) is an integral part of antenatal care, but issues related to supply, coverage and usability still remain.
It is increasingly being recognized that preventing anemia in adolescent girls and women of reproductive age will assure that their iron needs are met if and when these women become pregnant. Intermittent (e.g., once a week) IFA supplementation can be given to pubescent girls and menstruating women living in settings with an anemia prevalence of 20 percent or higher (WHO, 2011b).
In addition, WHO recommends intermittent iron supplementation of preschool (24–59 months) and school-age (5–12 years) children if anemia prevalence is higher than 20 percent. Daily iron supplementation is recommended for children 6–23 months in settings where the prevalence of anemia in children approximately one year of age is above 40 percent or where the diet does not include foods fortified with iron (WHO, 2015). Nevertheless, the safety of supplying more iron to children in malaria-endemic areas or where intestinal pathogenic bacteria are common is still a matter of concern.
Folic acid supplements are suggested prior to pregnancy to prevent the development of neural tube defects in the fetus; since the fetus’s neural tube develops in the first few weeks of pregnancy, waiting until a woman knows she is pregnant is typically too late to improve her intake of folate. This intervention is especially important when the diet is low in folate or fortification programs with folic acid are nonexistent in the area.
Calcium supplementation during pregnancy is a relatively new recommendation from the WHO to reduce the risk of eclampsia (WHO, 2013). Experience in the use of this intervention is low, and programmatic issues related to its demand, use and adherence still have to be resolved.
Vitamin A supplementation is given biannually to children aged 6 months to 5 years old as part of child health days or campaigns in many countries. As vitamin A can be stored in body organs up to 4–6 months, this intervention has been demonstrated as efficacious and practical (Edejer, et al., 2005). In the event that other interventions supplying vitamin A are already occurring in a population, adjustment to the supplementation programs might be needed in order to prevent excess supplementation.
2. Point-of-Use “Fortification”
Multiple micronutrient powders (MNP) are supplements in the form of single-use packets of powder containing vitamins and minerals that can be added to any semi-solid food. They are targeted to children aged 6–23 months. Formulations of MNP containing iron, zinc and vitamin A have been suggested by WHO as an intervention to reduce anemia when the prevalence in children is higher than 20 percent (WHO, 2011a). Other micronutrients may be incorporated into the MNP depending on the identified micronutrient inadequacies of the target group. Because these supplements are added to semi-solid foods for immediate consumption, the practice is referred to as “point-of-use fortification” or “home fortification.”
While studies suggest that MNPs are as efficacious as iron drops in reducing and preventing anemia (De-Regil, et al., 2011), MNPs should not replace already well-functioning supplementation programs, such as vitamin A and iron programs, unless results from feasibility, programmatic-efficiency and acceptability studies indicate that MNPs will have similar or better population coverage and will perform significantly better than existing programs.
Some of the factors to consider before adopting the use of MNPs include whether the product will be imported or produced in-country and whether a custom formulation can be adopted. A successful MNP program needs to implement MNPs within the context of improving infant and young child feeding practices; it also must include a strong behavior change communication component to ensure effective use and adherence. Experience is limited in using MNPs at scale, and the sustainability of using these products in large programs has yet to be established.
II. Selecting One or More Micronutient Interventions
A five-step process can be used to decide whether to implement one or more micronutrient interventions (Box 4). This process is necessary to ensure that newer programs are in line with the aims and objectives of the broader national nutrition agenda. These steps provide information on how best to integrate newer programs into existing systems.
1) Identify the Problem:Assessing micronutrient consumption and the sources of micronutrients from the diet is a key first step. Both quantitative and qualitative data (where available) should be used to determine the type of deficiency that exists, the prevalence in the targeted population and its severity. It is also important to identify the main risk factors (dietary, social, health, environmental, etc.) influencing the problem and the range of interventions that can be used to address the context-specific situation.
Dietary consumption surveys can estimate micronutrient intakes and predict main inadequacies. Countries are increasingly undertaking micronutrient surveys to collect population-level data on micronutrient status to use in setting targets for and tracking nutrition programs. The most commonly measured micronutrients are iron, zinc, vitamin A, vitamin B12, folate and zinc, along with markers of inflammation, to help interpret micronutrient markers. Recently, the assessment of vitamin D has been introduced, as in many communities the exposure of skin to sunlight is insufficient for the body to synthesize this nutrient.
Multiple micronutrient deficiencies frequently coexist. When data are scarce, the prevalence of some of the easier-to-measure micronutrient markers can be used as a proxy for the prevalence of deficiencies of other markers. For example, if iron deficiency is detected, zinc deficiency is highly probable.
Box 4. Selecting the Micronutrient Intervention
- Identify the problem: Evaluate the type, prevalence and severity of deficiencies and identify target population.
- Establish a multi-sectoral platform: Involve different stakeholders in defining the long-term and short-term goals before implementing the intervention and in conducting an analysis of current programs to identify the gaps in micronutrient intake and status.
- Consider safety: Assess how to implement one or more interventions to augment current intakes to a safe level.
- Identify delivery systems: Evaluate potential enabling factors and barriers to implementing programs using the newly identified delivery systems.
- Develop monitoring and evaluation plan: Designed alongside the intervention, it will allow for midcourse corrections and provide information on the impact of the intervention.
2) Establish a Multi-sectoral Platform: All interventions that have been described in the sections above work best in coordination with an integrated plan of action for micronutrients. Ideally, multiple sectors would work together to identify the problem. Subsequently, there should be involvement from all stakeholders to define the long-term and short-term program goals before implementing the selected intervention(s). The micronutrient program selected for implementation should have a clear focus, with a plan and timeline that are in sync with existing programs. This, too, helps in mapping current programs, where the interventions and the amount of micronutrients that are being delivered through different micronutrient vehicles are summarized.
3) Consider Safety: The assessment of the potential for one or more interventions to augment current intakes to amounts that may be risky is an important indicator of the safety of programs being considered. Data on consumption patterns can be incorporated into this step as well, and program managers should evaluate when the supply of micronutrients is sufficient and whether the intake of one or more micronutrients from all sources exceeds the tolerable Upper Intake Levels (UL), which may result in adverse effects over the long term. These considerations should feed back into the delivery systems being selected in the next step. Nutrient-infection and drug-nutrient interactions should be carefully considered as well. For example, programs that use supplements containing iron should be implemented in conjunction with malaria control and prevention measures (WHO, 2015).
4) Identify Delivery Systems: The following components of a delivery system should be considered: platform, supply chain, social and behavior change communication plan, available resources and human and institutional capacity, with clearly defined roles and responsibilities. It is necessary to evaluate enabling factors and barriers to implementing programs using the newly identified delivery systems. The programs within the different sectors and the delivery vehicles used are important inputs into deciding whether the intervention(s) under consideration are appropriate in conjunction with existing programs.
5) Develop Monitoring and Evaluation Plan: Monitoring and evaluation plans for the intervention should be designed alongside the implementation plan. Monitoring systems send regular and timely information to program managers to foresee barriers to implementation and design course correction for program improvements. Evaluation of the interventions provides feedback on whether the delivery of micronutrients had the intended impact on the population. The monitoring and evaluation systems should be simple and integrated into the regular flow of information from the health or other sectoral systems. In addition, these systems should document results and allow for their dissemination to policymakers and beneficiaries alike to ensure sustainability.
Conclusion
There is a wide array of interventions available to tackle micronutrient inadequacies. For the long-term, interventions aimed toward increasing dietary diversification should be the central component of micronutrient deficiency prevention and control efforts. It must be recognized that these interventions will take time to show impact, and they might not provide the required amounts of all nutrients needed throughout the lifecycle. Until populations’ diets improve, and to meet the deficiencies that longer-term interventions will correct, food fortification and supplementation remain the primary sources for delivering key micronutrients.
While most of the results of published studies within public health literature point to the success of food fortification and supplementation programs, many of them come from efficacy trials where the quality of the vehicle and adherence to the treatment are being assured. These conditions of quality and adherence are rarely encountered in real program settings. Therefore, attention to the programmatic issues that determine feasibility and performance of the interventions must be taken into consideration. Selection of one or more of these interventions should employ a situation assessment, including an understanding of the existing health and nutrition interventions in country, the availability of resources, safety considerations and human and infrastructure capacity.
References
Allen, L. H. (2005). Multiple micronutrients in pregnancy and lactation: An Overview. The American Journal of Clinical Nutrition, 81(5): 1206s–1212s.
Andersson, M., Vallikkannu, K., & Zimmermann, M.B. (2012). Global iodine status in 2011 and trends over the past decade. The Journal of Nutrition, 142(4): 744–750. doi: 10.3945/jn.111.149393.
Arroyave, G., Mejía, L. A., & Aguilar, J. R. (1981). The effect of vitamin a fortification of sugar on the serum vitamin a levels of preschool Guatemalan children: a longitudinal evaluation. The American Journal of Clinical Nutrition, 34(1): 41–9.
Black, R. E. (2014). Global distribution and disease burden related to micronutrient deficiencies. Paper presented at Nestlé Nutrition Institute Workshop, Muscat, Oman.
Copenhagen Consensus Center. (2012). Expert panel findings [PDF, 457KB]. Copenhagen, Denmark: Copenhagen Consensus Center.
De-Regil, L. M., Suchdev, P. S., Vist, G. E., Walleser, S., & Peña-Rosas, J. P. (2011). Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD008959.pub2.
Dewey, K. G., & Adu-Afarwuah, S. (2008). Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal &.Child Nutrition, 4(Suppl 1): 24–85. doi: 10.1111/j.1740-8709.2007.00124.x.
Edejer, T. T., Moses Aikins, M., Black, R., Wolfson, L., Hutubessy, R., & Evans, D. B. (2005). Cost effectiveness analysis of strategies for child health in developing countries. BMJ, 331: 1177.
Eichler, K., Wieser, S., Rüthemann, I., & Brügger, U. (2012). Effects of micronutrient fortified milk and cereal food for infants and children: a systematic review. BMC Public Health, 12: 506. doi:10.1186/1471-2458-12-506.
Fiedler, J. L., & Lividini, K. (2014). Managing the vitamin A program portfolio: a case study of Zambia, 2013-2042. Food and Nutrition Bulletin, 35(1): 105–25.
Fiedler, J. L., Lividini, K., & Bermudez, O. I. (2015). Estimating the impact of vitamin A-fortified vegetable oil in Bangladesh in the absence of dietary assessment data. Public Health Nutrition, 18(3):414–20. doi:10.1017/S1368980014000640.11.
Food and Drug Administration (FDA). Dietary supplements. Last updated April 2018.
Gibson, R. S. (2014). Enhancing the Performance of food-based strategies to improve micronutrient status and associated health outcomes in young children from poor-resource households in low-income countries: challenges and solutions. In Improving Diets and Nutrition: Food–based Approaches, edited by Brian Thompson and Leslie Amoroso, 19–31. Boston, MA, USA: CAB International and Rome, Italy: Food and Agriculture Organization (FAO) of the United Nations.
Gibson, R. S., Perlas, L., & Hotz, C. (2006). Improving the bioavailability of nutrients in plant foods at the household level. Proceedings of the Nutrition Society, 65(2):160–8.
Gibson, R. S., & Anderson, V. P. (2009). A review of interventions based on dietary diversification or modification strategies with the potential to enhance intakes of total and absorbable zinc. Food and Nutrition Bulletin, 30(1 Suppl): S108–43.
Guldan, G. S., Fan, H. C., Ma, X., Ni, Z. Z., Xiang, X., & Tang, M. Z. (2000). Culturally appropriate nutrition education improves infant feeding and growth in rural Sichuan, China. The Journal of Nutrition, 130(5):1204–11.
HarvestPlus (2012). Biofortification: improving nutrition through agriculture [Powerpoint slides]. Presentation by Fabiana Moura, HarvestPlus Nutritionist.
Herforth, A., & Harris, J. (2014). Understanding and applying primary pathways and principles. brief #1 [PDF, 1.4MB]. Improving Nutrition through Agriculture Technical Brief Series. Arlington, VA, USA: USAID/Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) Project.
Hertrampf, E., Cortés, F., Erickson, J. D., Cayazzo, M., Freire, W., Bailey, L. B., … Pfeiffer, C. (2003). Consumption of folic acid-fortified bread improves folate status in women of reproductive age in Chile. The Journal of Nutrition, 133(10):3166–69.
Horton, S., Mannar, V., & Wesley, A. (2008). Best practice paper: micronutrient fortification (iron and salt iodization) [PDF, 750KB]. Copenhagen, Denmark: Copenhagen Consensus Center.
Hotz, C., Loechl, C., Lubowa, A., Tumwine, J. K., Ndeezi, G., Masawi, A. N. … Gilligan, D. O. (2012). Introduction of beta-carotene-rich orange sweet potato in rural Uganda resulted in increased vitamin A intakes among children and women and improved vitamin A status among children. The Journal of Nutrition, 142:1871–80.
Imdad, I., Yakoob, M.Y., & Bhutta, Z.A. (2011). The effect of folic acid, protein energy and multiple micronutrient supplements in pregnancy on stillbirths. BMC Public Health 11(3): S4.
Kodkany, B. S., Bellad, R. M., Mahantshetti, N. S., Westcott, J. E., Krebs, N. F., Kemp, J. F., & Hambidge, K. M. (2013). Biofortification of pearl millet with iron and zinc in a randomized controlled trial increases absorption of these minerals above physiologic requirements in young children. The Journal of Nutrition, 143: 1489–93. doi: 10.3945/jn.113.176677.
Lönnerdal, B. (1985). Biochemistry and physiological function of human milk proteins. The American Journal of Clinical Nutrition, 42(6): 1299–1317.
Martorell, R., Ascencio, M., Tacsan, L., Alfaro, T., Young, M. F., Addo, O. Y., Dary, O., & Flores-Ayala, R. (2015). Effectiveness evaluation of the food fortification program of Costa Rica: impact on anemia prevalence and hemoglobin concentrations in women and children. The American Journal of Clinical Nutrition, 101: 210–7. doi:10.3945/ajcn.114.097709.
Mayo-Wilson, E., Imdad, A., Herzer, K., Yakoob, M. Y., & Bhutta, Z. A. (2011). Vitamin A supplements for preventing mortality, illness, and blindness in children aged under 5: systematic review and meta-analysis. BMJ, 343:d5094.
Nutrition Service of the World Food Program. (2006). Micronutrient fortification: WFP experiences and ways forward. Food and Nutrition Bulletin, 27(1): 67–75.
Peña-Rosas, J. P., De-Regil, L. M., Dowswell, T., & Viteri, F. E. (2012). Daily oral iron supplementation during pregnancy (review). Cochrane Database of Systematic Reviews. doi: 10.1002/14651858.CD004736.pub4.
Petry, N., Egli, I., Gahutu, J. B.,Tugirimana, P. L., Boy, E., & Hurrell, R. (2014). Phytic acid concentration influences iron bioavailability from biofortified beans in Rwandese women with low iron status. The Journal of Nutrition, 144:1681–87. doi: 10.3945/jn.114.192989.
Torheim, L. E., Ferguson, E. L., Penrose, K., & Arimond, M. (2010).Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. The Journal of Nutrition, 140(11):2051S–8S. doi: 10.3945/jn.110.123463.
von Grebmer, K., Saltzman, A., Birol, E., Wiesmann, D., Prasai, N., Yin, S., … Sonntag, A. (2014). 2014 global hunger index: the challenge of hidden hunger. International Food Policy Research Institute.
Webb, P., Rogers, B., Rosenberg, I., Schlossman, N., Wanke, C., Bagriansky, J., Sadler, K. … Narayan, A. (2011). Improving the nutritional quality of U.S. food aid: recommendations for changes to products and programs [PDF, 4.2MB]. Boston, MA, USA: Tufts University.
World Health Organization (WHO). (2011a). Guideline: use of multiple micronutrient powders for home fortification of foods consumed by infants and children 6-23 months of age [PDF, 606MB]. Geneva, Switzerland: WHO.
——. (2011b). Guideline: intermittent iron and folic acid supplementation in menstruating women [PDF, 1.2MB]. Geneva, Switzerland: WHO.
——. (2013). Guideline: calcium supplementation in pregnant women. Geneva, Switzerland: WHO.
——. (2015). Iron supplementation in children 6-23 months of age. Geneva, Switzerland: WHO.
WHO and FAO. (2004). Vitamin and mineral requirements in human nutrition [PDF, 2.1MB]. Geneva, Switzerland: WHO and Rome, Italy: FAO.
——. (2006). Guidelines on food fortification with micronutrients. Geneva, Switzerland: WHO and Rome, Italy: FAO.
——. (2015). Codex Alimentarius International Food Standards: general principles for the addition of essential nutrients to foods, revised version.[PDF, 147KB]
This Technical Brief will be periodically updated. Comments from readers are welcome to Leslie Koo, especially comments to help clarify the information provided or where additional information may be useful.
Footnotes
1 Nutrition-Sensitive Agriculture: Nutrient-Rich Value Chains
2 Nutrition-Sensitive Agriculture: Applying the Income Pathway
3 When the product name includes “Plus”, it means that the product has been enhanced with additional micronutrients.

Comment
Make a general inquiry or suggest an improvement.